Degenerative disc disease is a condition where the intervertebral discs, acting as a cushion between spine vertebrae, deteriorate.
Tendons are connective tissues that consist of collagen and connect muscles and bones. They are strong and fibrous, but although they can tolerate stress, they are not unbeatable.
Artificial disc replacement, which is also called vertebral disc arthroplasty, spine arthroplasty or total disc replacement, is a kind of spine surgery that replaces a damaged intervertebral disc with an artificial one. A skilled spine surgeon replaces the affected disc with a metal or metal and plastic device in between the vertebrae. The main aim of artificial disc replacement is getting relief from chronic back pain, restoring disc height, and maintaining spinal flexibility. It is also one of the best alternatives to spinal fusion surgery.
How does artificial disc replacement surgery work?
Most spine surgeons today prefer artificial disc replacement because it is minimally invasive. Here, rather than making an incision in the neck or back, the spine surgeons make tiny incisions in the front part of the body. Then the internal organs are slowly moved to the side to assess the affected disc. This method does not require cutting the muscles, resulting in reduced pain and fast recovery.
After removal of the problematic disc, the lower and upper joint plates are fixed to the spinal endplate bones at the upper edge and lower edge of the damaged disc level. When those plates are in place, the surgeon puts a central core, whose design varies greatly based on different disc implant brands.
While in some, the plates and the core are inserted as one unit, in others, there will be a need to insert the core separately. The function of the central core is to allow movement in between the plates, facilitating bending of the spine and making the spine flexible like a normal disc.
There are several types of artificial disc replacements, and your spine surgeon might modify your vertebral bones present above and below the disc that is removed. With modification, the artificial disc is fixed in a precise position on your spine.
Artificial disc replacement for treating a single level of disease takes somewhere between 45 and 1.15 hours. There might be a requirement to take opioids in lower doses during the initial days of recovery. However, for most people, it’s possible to treat post-surgery discomfort by using acetaminophen, naproxen or th ibuprofen.
Who needs artificial disc replacement?
Artificial disc replacement is suitable for those who have the following conditions:
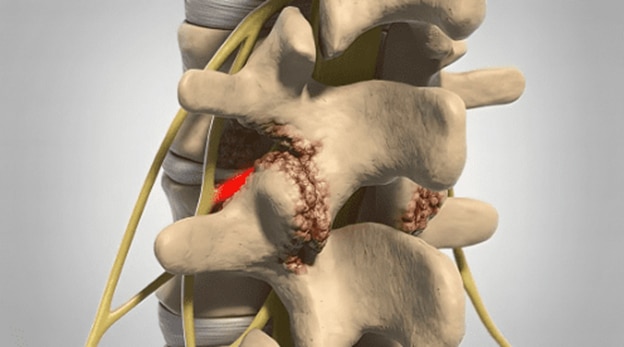
Degenerative disc disease
It is the natural wear and tear occurring in the intervertebral disc because of aging, physical stress and repetitive movement.
Herniated disc
It is also called bulging disc or protrusion of disc. Here the intervertebral disc lengthens beyond its usual space in the spine. It sometimes pushes into the spinal canal, thereby pinching the nerve present in the lower back or neck, causing back pain or neck pain.
Spinal stenosis
It is narrowing down the spinal canal that decreases the space of the spinal cord or the spinal nerve roots.
Conclusion
Artificial disc replacement is one of the advanced outpatient surgeries where the patients are not required to stay in the hospital. It is important to follow all post-surgery instructions and limit your day-to-day activities for a fast recovery. Physical therapies also help in healing fast and correctly and get all the benefits of artificial disc replacement.
For enquiries and online appointments:
Email – Naveen.st@gmail.com
Call/Whatsapp – +91 7676090119
Visit www.NaveenSpine.com to know more
Whiplash injury is a condition that occurs when suddenly moving your neck causes your cervical spine and the upper spine to move in ways leading to injury or neck sprain.
A vertebral column resection or VCR is a kind of osteotomy that is performed for correction of severe spinal deformity. Osteotomy is removal of bone, but in the case of VCR, it is one step further, where the doctor removes or resects one or multiple vertebrae from your spine.
Coccydynia is a medical term that refers to pain occurring in the coccyx region, that is tailbone pain. It is also referred to as coccygodynia, coccalgia, neuralgia or coccygeal.
Nowadays, people are working non-stop in front of computers for long periods and living a sedentary lifestyle where there are minimal activities, lack of exercises and bad food habits.
A spine disorder is a spine abnormality that can occur in any part of the spine, starting from the neck to the lower back. Because the spinal column is the primary support of your body and gives protection to your spinal cord, any disorder in your spine causes pain and in some cases becomes degenerative.
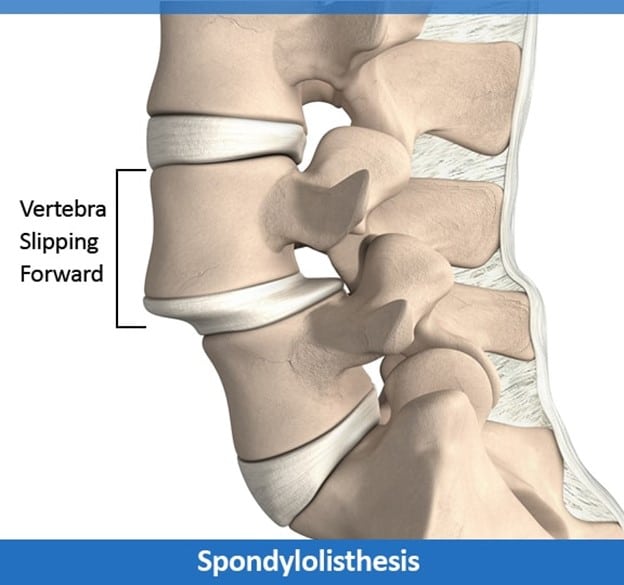
Spondylolisthesis is a condition in which one spinal bone slips from its place and is positioned on the top of the spinal bone present next to it. It commonly happens at the spinal base or the lumbar spine and is called spondylolisthesis of the lumbar spine.
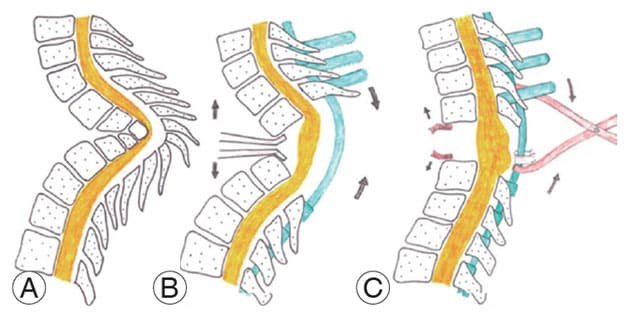
The spinal or vertebral system of a human being is amazing; it is perfectly balanced classically and forms the main support system of the whole body. It is slightly curved, forming an S-shape, thus balancing your neck, lower back, pelvis, and chest to keep your head, trunk, and legs in alignment.