Scoliosis is a condition where the spine bends sideways and sometimes twists, affecting individuals at any age and often forming an “S” or “C” shape. While many people associate scoliosis with teenagers, it can actually affect people of all ages, from infants to older adults. Recognizing the type of scoliosis is important because it helps guide treatment and management decisions.
Idiopathic Scoliosis
Idiopathic scoliosis is the most common type, making up about 80% of all cases. The word “idiopathic” indicates that the cause cannot be identified. This form of scoliosis often appears during growth spurts in children and adolescents, especially among girls. Idiopathic scoliosis is further divided based on age:
- Infantile (0–3 years): Rare, often noticed by parents or during routine check-ups.
- Juvenile (4–10 years): Less common, but early detection is important.
- Adolescent (11–18 years): The most frequent form, especially in teenage girls.
- Adult idiopathic: Sometimes, scoliosis that began in adolescence continues or progresses into adulthood.
Degenerative (Adult) Scoliosis
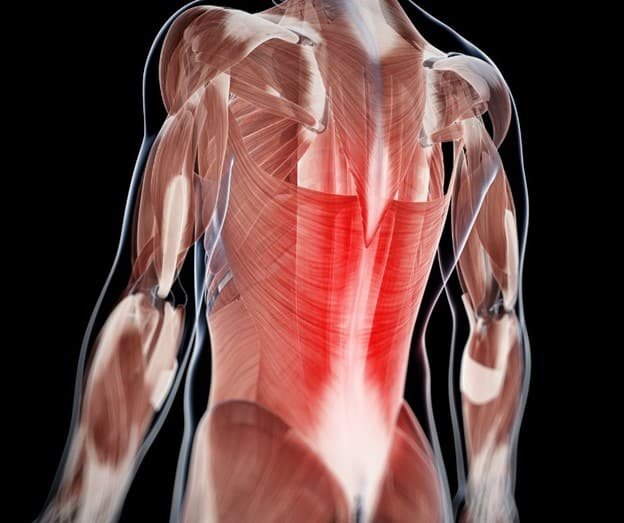
Degenerative scoliosis develops later in life, usually after age 50. With aging, wear and tear on the spine’s discs and joints can cause uneven changes that make the spine bend. This type typically involves the lower back and may bring symptoms such as discomfort, reduced flexibility, and difficulty standing straight. Degenerative scoliosis can develop on its own or as a progression of earlier scoliosis.
Congenital Scoliosis
Congenital scoliosis is a spinal condition present at birth, caused by abnormal formation of the vertebrae during fetal development. These spinal irregularities can lead to a sideways curve that may become more noticeable as the child grows. Although rare, this condition is sometimes detected in infancy or early childhood. It may be associated with other health conditions or organ development issues.
Neuromuscular and Syndromic Scoliosis
Some types of scoliosis are linked to underlying medical conditions:
- Neuromuscular scoliosis arises from diseases affecting the muscles or nerves, such as cerebral palsy, muscular dystrophy, or spinal muscular atrophy, which weaken the support around the spine. These conditions can make it harder for the muscles to support the spine, leading to more severe and rapidly progressing curves.
- Syndromic scoliosis occurs as part of certain genetic syndromes, such as Marfan syndrome or neurofibromatosis.
Functional (Non-Structural) Scoliosis
Unlike the other types, functional scoliosis is not caused by changes in the structure of the spine. Instead, it is usually due to temporary factors like differences in leg length or muscle spasms. Once the underlying cause is treated, the curve often disappears.
Why Knowing the Type Matters
Understanding the type of scoliosis is important for several reasons:
- Diagnosis: Different types require different tests and monitoring.
- Treatment: Options may include observation, physical therapy, bracing, or surgery, depending on the type and severity.
- Prognosis: Some forms progress rapidly and need early intervention, while others may remain stable for years.
Conclusion
Scoliosis is not a one-size-fits-all condition. It comes in several forms, each with its own causes and characteristics. Early detection and understanding the specific type of scoliosis are key to choosing the best treatment and achieving the best possible outcome. If you or your child has been diagnosed with scoliosis, talk to your orthopaedic specialist about which type you have and what treatment options are available.
For enquiries and online appointments:
Email – Naveen.st@gmail.com
Call/Whatsapp – +91 7676090119
Visit www.NaveenSpine.com to know more