
Spinal Stenosis Treatment in Bangalore
Spinal stenosis is one of those conditions that affects millions worldwide, actually—causing pain and mobility issues that can really disrupt a person’s day-to-day life. If you’re in Bangalore and looking for real expertise, you’ve got access to some advanced treatment options and specialists who genuinely get how complicated this can be.
Dr. Naveen Tahasildar stands out as one of the best spine specialist in Bangalore, bringing over 17 years of hands-on experience to the table. He offers a full range of spinal stenosis treatments, from conservative care to complex surgeries. His skillset covers everything from minimally invasive procedures and deformity corrections to spinal tumour surgeries, making him a go-to for patients not just in Bangalore, but across India.
If you are someone who is considering treatment for spinal stenosis, keep reading to find out the different treatments, success rates, and, let’s be honest, the costs involved. It helps to know your choices, whether you’re hoping to avoid surgery or you’re considering the latest techniques, and to weigh things like recovery time and what your long-term outlook might be before jumping in.
Early intervention is of utmost importance. Book your appointment today for a quick consultation and check-ups.
Understanding Spinal Stenosis
Spinal stenosis happens when the spaces in your spine start to narrow, squeezing the spinal cord and nerves. It’s especially common if you’re over 50, and it can really put a dent in your ability to move around or just enjoy life.
Definition and Causes of Spinal Stenosis
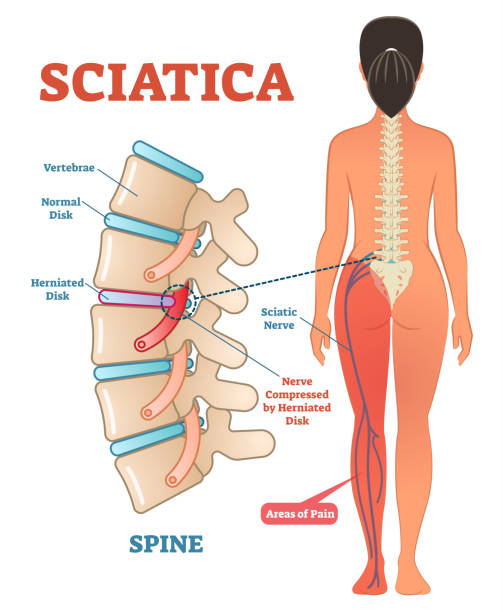
Basically, spinal stenosis means the spaces in your spinal column are shrinking. That puts pressure on the cord and the nerve roots running through your back.
Most of the time, it’s your lower back (lumbar spine) or neck (cervical spine) that gets hit. When those areas tighten up, you’re likely to feel pain, numbness, and have trouble moving normally.
Main Causes Include:
- Age-related degeneration – Just the usual wear and tear as we get older
- Arthritis of the spine – Inflammation leads to bone spurs
- Thickened ligaments – Ligaments stiffen and bulge into the canal
- Herniated discs – Discs get damaged and press on the nerves
- Bone spurs – Extra bone growth, usually from arthritis
Some folks are just born with a narrower canal, so congenital factors play a part too. And while it’s rare, spinal tumours can also press into the canal and cause problems.
It’s worth noting: this isn’t like scoliosis, which is about your spine curving. Stenosis is all about those spaces getting tighter inside your vertebrae.

Common Symptoms and Warning Signs
Symptoms usually sneak up slowly and get worse over time. Where the stenosis is located will drive which symptoms you notice the most.
Lumbar stenosis symptoms:
- Lower back pain that ramps up when you walk
- Leg pain, numbness, or weakness
- Pain eases up if you sit or lean forward
- Trouble walking long distances
Cervical stenosis symptoms:
- Neck pain and stiffness
- Numbness in your hands or arms
- Balance gets shaky
- Weakness in your hands—fine motor skills can take a hit
A lot of people notice that sitting or bending forward gives them some relief. It’s because that position opens up the spinal canal a bit, taking pressure off the nerves.
Warning signs you shouldn’t ignore:
- Sudden, severe weakness
- Losing control over your bladder or bowels
- Major balance issues
- Numbness spreading in your arms or legs
If you notice any of these, it could point to spinal cord injury—don’t wait, get checked out right away. Early treatment can stop things from getting worse and protect your nerves.
Risk Factors Associated With Spinal Stenosis
There are a bunch of things that can up your risk for spinal stenosis. Age is the big one—most people who get it are over 50.
Lifestyle factors matter too:
|
Category |
Specific Factors |
|
Age-related |
Disc degeneration, arthritis setting in |
|
Genetic |
Family history, or just being born with a narrow canal |
|
Medical conditions |
Osteoarthritis, rheumatoid arthritis |
|
Previous injuries |
Old spinal fractures, herniated discs |
If you’ve had spinal disc surgery before, the risk goes up. Scar tissue, or degeneration near the old surgery site, can make the canal even narrower.
Some of the main risk factors:
- Sitting around too much—muscles get weak
- Jobs that have you bending over and over again
- Old injuries or accidents involving your spine
- Carrying extra weight puts more strain on your back
Some medical issues can speed things up, like Paget’s disease (which messes with bone growth) or achondroplasia (which means you’re born with a narrow canal).
Most orthopedics experts will tell you: spotting risks early means you can do something about it. Regular exercise, good posture, and keeping your weight in check can slow things down if you’re prone to stenosis.
Wondering what really triggers this painful condition…? Let’s explore the root causes next.
Diagnosis and Evaluation - What’s The Procedure?
Getting spinal stenosis diagnosed properly means a thorough clinical check-up, plus some high-tech imaging. In Bangalore, top spine surgeons use detailed protocols to figure out exactly where, how bad, and why your spinal canal is narrowing.
Initial Clinical Assessment and Patient History
Everything starts with a deep dive into your medical history. Most patients show up with classic symptoms: leg pain when walking, numbness, and feeling better when sitting or leaning forward.
The physical exam zeroes in on your nerves. Key things they’ll check:
- How strong your muscles are
- Your reflexes
- What you can feel—sensory testing
- How you walk
The “shopping trolley test” is surprisingly telling. If you can walk farther while leaning on a trolley than standing straight, that’s a pretty good hint it’s spinal stenosis and not a blood flow issue.
How long you’ve had symptoms and how fast they’re getting worse are both big clues. Chronic symptoms over months or years usually mean degeneration, while sudden issues might point to something else.
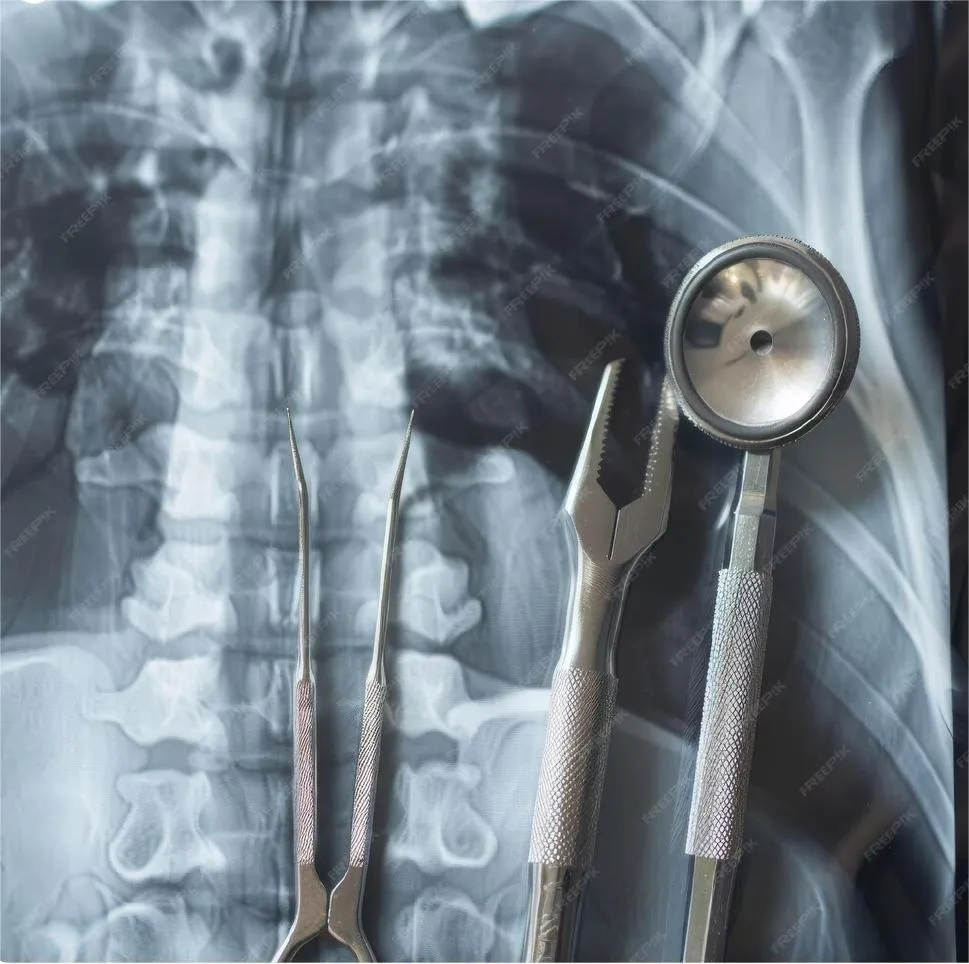
Diagnostic Imaging and Advanced Techniques

MRI scans are the go-to in Bangalore for diagnosing spinal stenosis. They’re non-invasive and offer a clear look at soft tissues—great for spotting herniated discs or thickened ligaments.
If the MRI is fuzzy or you can’t get one, CT myelography is next best. It’s especially good for bone detail.
X-rays help spot things like:
- Misaligned vertebrae
- Bone spurs
- Joint wear and tear
- Instability in the spine
Sometimes they’ll do dynamic X-rays—having you bend or extend—to see if your vertebrae are moving oddly, which could be part of the problem.
Places like Sparsh Hospital, Vasanth Nagar & At Dr. Naveen’s own clinic at Infantry Road have high-res imaging that can measure exactly how narrow things are and how much your nerves are getting squeezed. It’s pretty impressive, honestly.
Identifying Severity and Individualised Planning
Severity matters when it comes to treatment. If your canal is over 12mm wide (mild), you might do fine with conservative care. If it’s less than 8mm (severe), surgery could be on the table.
But it’s not just the images—doctors look at how your symptoms match up with what they see. Some folks have a really tight canal but barely notice, while others with moderate narrowing are miserable.
Functional scales help measure how much your symptoms mess with your life. Tools like the Zurich Claudication Questionnaire or Oswestry Disability Index are pretty standard for this.
If you’ve got multi-level stenosis, each spot gets checked out. Treatment priorities come down to:
- How bad your symptoms are at each level
- How tight the narrowing is
- Whether there’s instability
- Your overall health
Doctors will tailor the plan to your age, activity level, and other health issues. No cookie-cutter solutions here—each patient gets a custom approach for the best chance at a good outcome.
So how do you know if what you’re feeling is sciatica or just ordinary back pain? Let’s find out.
Dr. Naveen Tahasildar: Profile and Credentials
Dr. Naveen Tahasildar, a leading spine surgeon in Bangalore holds an MBBS and MS in Orthopaedics from the well-respected Post Graduate Institute of Medical Education and Research, Chandigarh, plus several international fellowships. Over the past 17+ years, he’s handled more than 3,000 complex spine surgeries at SPARSH Hospital in Bangalore.
Professional Education and Fellowships
He earned his MBBS and MS in Orthopaedics at PGIMER, Chandigarh—one of India’s top medical schools, and yes, it’s tough to get in.
Internationally, he did AO Spine Fellowship at Amrita Institute of Medical Sciences, Kochi, splitting time between neurosurgery and orthopaedics for a broad spine surgery experience.
He also completed an Orthopaedic Fellowship at Epworth Hospitals, Melbourne, learning from Mr. Marinis Pirpiris and spine surgeon Mr. David de La Harpe, focusing on diagnosing and treating degenerative spine issues.
Dr. Tahasildar was awarded a SICOT Travelling Fellowship at Aarhus University Hospital in Denmark, working under Professor Cody Bunger. He’s also been an Orthopaedic Trauma Fellow at Queen Elizabeth Hospital, Hong Kong.

Clinical Experience and Track Record
Since January 2014, Dr. Tahasildar has been the Consultant Spine Surgeon at SPARSH Hospital, running the spine unit on his own.
He’s handled everything from the cervical spine down to the sacrum—over 100 scoliosis corrections in the past eight years, including some pretty complex cases.
He’s a member of:
- AO Spine
- Association of Spine Surgeons of India (ASSI)
- North American Spine Society (NASS)
- Bangalore Orthopaedic Society
- Indian Orthopaedic Association
- Karnataka Orthopaedic Association
- SICOT
He’s published 28 research papers (cited 256 times), reviews for top spine journals, and has written chapters for medical textbooks. Clearly, he’s not just a surgeon—he’s an academic, too.
Non-Surgical Treatment Options
For a lot of people with spinal stenosis, conservative treatments can make a big difference, especially when it comes to pain and getting back to normal activities. These non-surgical options are usually the first thing doctors try before talking surgery.
Medications and Pain Management
NSAIDs (non-steroidal anti-inflammatory drugs) are the mainstay for pain. Stuff like ibuprofen and naproxen help cut down inflammation and take the edge off pain around those pinched nerves.
Muscle relaxants can be useful if you’re getting muscle spasms along with your back pain. They help loosen things up so you can move better.
For nerve pain that feels like shooting or burning, neuropathic medications (like gabapentin or pregabalin) are often prescribed. They’re pretty effective for those weird, electric-type pains in your legs.
Corticosteroid injections go right into the epidural space to calm inflammation. For a lot of patients, these shots can bring months of relief—though, to be fair, it’s not a permanent fix.
Physiotherapy is a big deal in orthopedics. Tailored exercises strengthen your core, improve posture, and help you stay flexible. Physiotherapists usually put together a plan that focuses on gently extending your spine and easing pressure on the nerves. It’s not always easy, but it can really pay off.
Lifestyle Adjustments and Patient Education
Postural modifications can make a surprising difference in managing symptoms. Most patients quickly learn to steer clear of activities that really arch the spine—think standing around for ages or trekking downhill for too long. It’s not always easy, but a little awareness helps a lot.
Walking aids like frames or shopping trolleys aren’t just for show—they actually help folks keep a more comfortable posture, especially during errands or longer strolls. That slight forward lean they encourage? It often takes the edge off leg pain and that annoying numbness.
Weight management also plays a role. Shedding even a few kilos can ease pressure on the spine, which, in turn, might boost mobility. It’s not a magic fix, but it’s definitely worth considering.
Activity pacing is about knowing your limits—without giving up on staying active. It’s a bit of a balancing act: mixing up movement with rest, and not getting stuck in one position for too long (especially if it makes things worse).
Ergonomic adjustments—even small ones—can bring real relief. Higher chairs, propping up your knees while you sleep, or tweaking how you go about daily routines can all help keep stenosis symptoms at bay.
Surgical Interventions for Spinal Stenosis
If conservative treatments just aren’t cutting it, surgery sometimes becomes the next step for spinal stenosis. These days, spine surgery is all about decompressing pinched nerves while keeping the spine stable, and surgeons are leaning heavily on minimally invasive approaches whenever they can.
Minimally Invasive Spine Surgery
Minimally invasive spine surgery is honestly a big leap forward for patients with spinal stenosis. Instead of the old-school, big-incision approach, these techniques use tiny cuts and special tools to get the job done with less collateral damage.
Surgeons go in with endoscopic or microscopic tools through portals barely big enough for a finger. This means a lot less muscle trauma compared to traditional open surgery, which is a huge win for recovery.
Some of the main perks:
- Less blood loss during surgery
- Shorter hospital stays (sometimes just one night)
- Quicker recovery—think days, not weeks
- Lower infection risk
- Minimal scarring
Most people find they have less pain after surgery and can get back to their routines faster. The precision here lets surgeons target nerve compression without messing with healthy tissue around it.
For many, recovery is pretty swift—you might even go home the same day or after a quick overnight stay. Light activities are usually back on the table within a few days.
Spinal Fusion Techniques
Spinal fusion comes into play when decompression alone would leave the spine unstable. It’s basically joining two or more vertebrae together so they stop moving relative to each other.
Modern fusion uses bone grafts or synthetic stuff to help the bones grow together, and metal hardware (screws, rods, plates) keeps things steady while that healing happens.
Common fusion methods include:
- Posterior fusion – from the back
- Anterior fusion – from the front
- Lateral fusion – from the side
- Combined approaches – a bit of everything
It usually takes three to six months for the bones to fully fuse. The hardware keeps everything lined up in the meantime.
Fusion is often paired with decompression, so you get nerve relief and long-term stability in one go. It’s a comprehensive fix, though it does mean a longer recovery than decompression alone.
Getting back to normal is gradual—no heavy lifting or twisting until the fusion’s solid. Patience is key here.
Related Spinal and Orthopaedic Procedures
Dr. Naveen Tahasildar doesn’t just stick to spinal stenosis—his expertise covers spinal cord injury management, tricky deformity corrections, and advanced reconstructions. These areas often overlap, so patients with more than one musculoskeletal issue benefit from a coordinated approach.
Spinal Cord Injury Management
Spinal cord injuries demand both quick action and a long-haul recovery plan. Dr. Tahasildar handles everything from sudden trauma cases to the ongoing headaches of chronic spinal cord problems.
Acute injury management is all about stabilizing the spine fast and stopping further nerve damage. Sometimes, surgical decompression needs to happen within a day or two to give the best shot at recovery.
Chronic care means dealing with complications like spasticity, weird blood pressure swings, or new deformities. These patients need regular check-ins and tweaks to their treatment as things change.
Reconstruction procedures can restore some function if the initial healing didn’t go as hoped. Advanced options like nerve grafts, tendon transfers, or implant-based stabilization systems come into play here.
Scoliosis and Deformity Corrections
Scoliosis correction isn’t just for kids—adults with degenerative curves are in the mix too. Dr. Tahasildar does thorough assessments to pick the right surgical plan for each case.
Adolescent scoliosis usually gets treated with posterior spinal fusion and hardware. These days, the goal is to keep as much movement as possible while still correcting the curve.
Adult deformity correction is trickier, thanks to worn-out discs and weaker bones. These often need a combo of front-and-back approaches to get things straightened out.
Revision surgeries tackle problems from earlier operations or worsening deformities. These are no walk in the park—they call for serious expertise in complex reconstructions.
After surgery, close monitoring is crucial to catch any issues early and make sure the correction holds up. Regular follow-ups help keep things on track.
Book a consultation today to find out which treatment option suits you best.
Wondering what makes one clinic stand out from another for sciatica care? Here’s what to look for.
Cost of spinal stenosis surgery
The price tag for spinal stenosis surgery in Bangalore really depends on the procedure and how complicated things get. Laminectomy—which is the go-to for most cases—can run anywhere from ₹1,10,000 to ₹4,00,000. Not exactly pocket change, right?
The surgical method matters a lot for cost. Minimally invasive options usually cost more upfront, but you might save overall thanks to less time in the hospital.
What drives the cost?
- Hospital’s facilities and reputation
- Surgeon’s skill and experience
- Type of surgery you actually need
- How severe your stenosis is
- How long you’ll need to stay in the hospital
Consultation fees with spine specialists in Bangalore tend to land between ₹800 and ₹2,500. Pre-surgery tests will tack on another ₹2,800 to ₹8,000, depending on what’s needed.
| Cost Component | Range (₹) |
| Surgeon consultation | 800 – 2,500 |
| Diagnostic tests | 2,800 – 8,000 |
| Laminectomy surgery | 1,10,000 – 4,00,000 |
| Hospital stay | 20,000 – 50,000 |
Spinal decompression surgery for stenosis usually falls between ₹1,40,000 and ₹1,80,000. This covers procedures to remove bone spurs or tissue pressing on the spinal canal.
Don’t forget about extra costs: anesthesia, post-op meds, and physio sessions all add up. Private hospitals typically charge more than government ones, but you do get better amenities and less waiting around.
It’s smart to budget for follow-up visits and the possibility of complications, just to be on the safe side.
Success Rates of Spinal Stenosis Surgery
Spinal stenosis surgery generally shows success rates between 70% and 90%, though it really depends on the procedure and, honestly, where you’re getting it done. There’s a lot of variation—different hospitals, different surgeons, different patients. It’s not a one-size-fits-all situation.
Decompression surgery tends to have better outcomes, especially when it comes to easing leg pain and those annoying neurogenic claudication symptoms. Most people notice they can walk farther and feel less numbness within a few months, which is pretty encouraging if you ask me.
Doctors usually measure the success of spinal stenosis surgery by looking at a few things:
- Pain reduction in the legs and back
- Improved walking distance before symptoms kick in
- Better quality of life scores
- Less numbness and weakness overall
Who gets picked for surgery—patient selection criteria—makes a big difference. Folks who are really struggling with daily activities because of severe symptoms tend to see the most benefit. If your stenosis is pretty mild, the results might not be as dramatic.
Age and general health come into play, of course. Even so, a lot of older patients still see real improvements after surgery. On the flip side, things like diabetes or peripheral vascular disease can make recovery a little trickier.
Picking the right surgical technique matters a lot, too. Minimally invasive options can actually stack up pretty well against traditional open surgery, and you might bounce back a bit faster. Not bad, right?
Looking at the long-term, studies show symptom relief usually sticks around for most people for years after surgery. That said, some folks do have symptoms creep back in, often because the spine keeps degenerating at nearby spots.
Setting realistic expectations is key—if you go in thinking all your symptoms will vanish, you might be disappointed. But most people walk away with a lot less pain and a better ability to get around, which is really what matters in the end.
Spinal treatments need expertise and precise care. We at Dr. Naveen’s Spine & Ortho Clinic ensure your treatment & recovery both are seamless. Book your consultation today.
